Fall/Winter 24/25
Here we would like to provide you with up-to-date information and surveys from the RESPINOW project and other sources that allow the epidemiological situation and possible development with regard to the dynamics and disease burden of RSV, influenza and pneumococci.
Scenarios for RSV Dynamics in the 2024-2025 Season
Respiratory Syncytial Virus (RSV) poses significant risks, especially to infants and older adults. For the 2024-2025 season, interventions such as monoclonal antibodies for infants and vaccinations for older adults are essential to mitigate the impact of RSV. Scenario modelling helps estimate the effectiveness of these interventions in reducing RSV cases, transmission, and hospitalizations, aiming to improve models for research purposes. Results are subject to relevant uncertainties regarding the actual uptake of interventions as well as expected dynamics of the season and are presented here mainly to enable comparison with other modelling groups.
Overview of interventions
Two interventions were modelled with an existing RSV ODE model able to integrate (sentinel) surveillance and population-based data to explore their potential effects:
1. Monoclonal antibodies for infants (0-1 years):
Administering monoclonal antibodies aims to reduce severe RSV outcomes in the most vulnerable age group. This intervention is expected to decrease hospitalization rates by up to 80% among infants. A coverage rate is assumed to be between 60-80%, with a median estimate of 70%.
2. Vaccination for older adults (60+ years):
Vaccines for older adults aim to reduce hospitalizations by up to 90%. In addition, the vaccine is assumed to reduce transmission by approximately 80%. The vaccine is projected coverage of 30-50% and a median value of 43.3%, which is similar with influenza vaccine coverage. The dual benefit of vaccination, reducing hospitalizations and transmission, makes it a cornerstone of the intervention strategy.
Modeling scenarios
Two scenarios were designed to project RSV outcomes based on different intervention combinations:
Scenario 1:
◦ Monoclonal antibodies are administered to infants (0-1 years), achieving a substantial reduction in hospitalizations in this age group.
◦ Vaccination is provided to older adults, focusing on reducing hospitalizations.
Scenario 2:
◦ Similar to Scenario 1, monoclonal antibodies are deployed for infants, achieving a comparable reduction in hospitalization rates.
◦ Vaccination coverage expands among older adults, targeting both hospitalization and transmission reduction. The additional transmission reduction is anticipated to decrease overall RSV spread, further protecting vulnerable populations.
Results
• No intervention:
In which no intervention setting, RSV transmission follows typical seasonal patterns, with a high number of cases and hospitalizations, particularly among infants. This scenario underscores the need for proactive measures to reduce the impact of RSV (Figure 1).
• Scenario 1:
Monoclonal antibody use significantly reduces hospitalizations in infants by about 50%. While targeted vaccination in older adults effectively decreases severe outcomes in this group. However, without transmission reduction in vaccination, overall RSV cases remain high, so the indirect effect on the population is relatively limited (Figure 2)
• Scenario 2:
Scenario 2 combines the dual impact of vaccination on transmission and hospitalization. Reduced transmission rates reduce the spread of RSV across age groups, especially in the older adult group. The reduction in cases in the older age groups is above 50%. Hospitalization outcomes decreased dramatically in infants and older adults, comparable to scenario 1 (Figure 3).
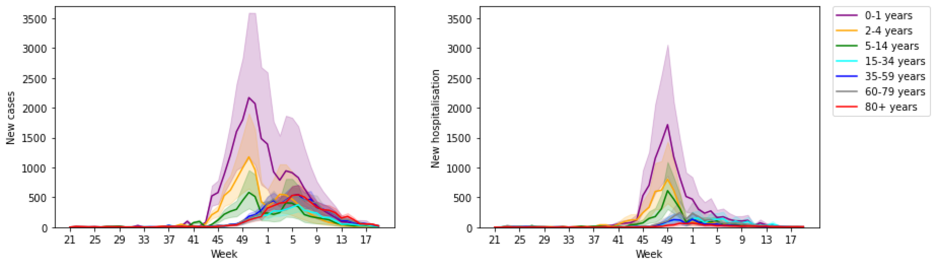
Figure 1: Estimated new RSV cases and hospitalizations for no intervention
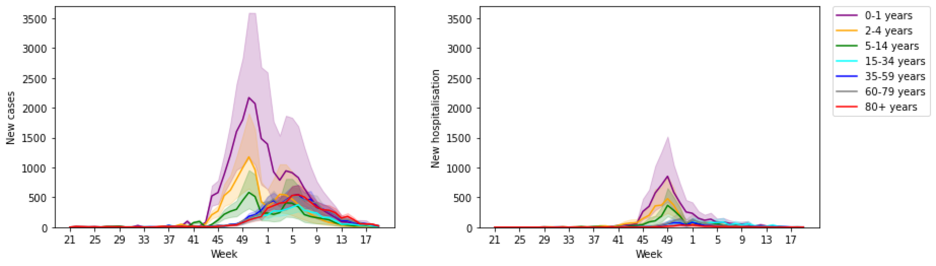
Figure 2: Estimated new RSV cases and hospitalizations for Scenario 1
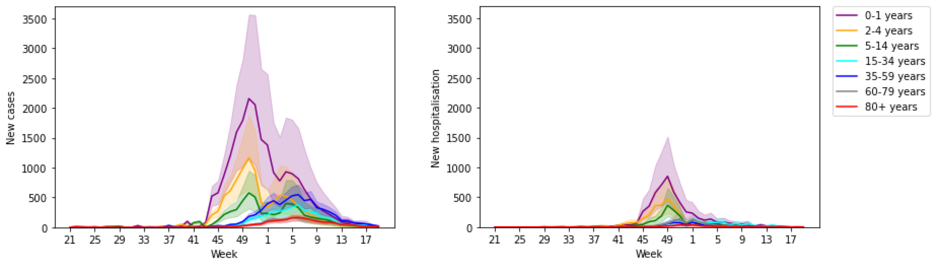
Figure 3: Estimated new RSV cases and hospitalizations for Scenario 2
Conclusion
The modelling results for the 2024-2025 RSV season emphasize the critical importance of targeted interventions. While monoclonal antibodies effectively protect infants from severe outcomes, vaccination programs for older adults offer the added benefit of reducing transmission, creating a cascading effect that protects the wider population. Public health efforts should prioritize achieving high coverage rates for both interventions to maximize their impact on hospitalizations and suppression of RSV throughout the population